Non-communicable diseases (NCDs) are increasingly becoming a public health challenge, particularly in resource-limited settings, where there is limited access to preventive care, early detection, and health literacy. Nevertheless, there is an immense potential of digital technologies to contribute to the enhancement of overall community health. Similarly, the WHO PEN Disease Interventions for Primary Healthcare in Low-Resource Settings has demonstrated evidence of improving NCD outcomes. Nevertheless, its effectiveness in the Indian settings has not been explored.
About the study
Non-communicable diseases (NCDs), also known as chronic diseases, tend to be of long duration and are the result of a combination of factors

Cardiovascular diseases

Chronic Respiratory Diseases
Diabetes
Cancer
What Are Non-Communicable Diseases (NCDs)?
- NCDs are medical conditions that are not caused by infectious agents and cannot be spread from one person to another.
- They are chronic diseases that usually last for a long time and progress slowly.
- Common examples include:
- Cardiovascular diseases such as heart attacks and strokes
- Diabetes mellitus
- Cancers (e.g., lung, breast, cervical)
- Chronic respiratory diseases like asthma and chronic obstructive pulmonary disease (COPD)
- Other significant conditions include mental health disorders, chronic kidney disease, and neurological disorders (WHO, 2025).
Risk Factors for NCDs
- Tobacco use: Smoking and tobacco chewing increase risks, especially for lung cancer, heart disease, and COPD.
- Unhealthy diet: High intake of salt, sugar, saturated fats, and low fruit and vegetable consumption.
- Physical inactivity: Sedentary lifestyle contributes to obesity, hypertension, and insulin resistance.
- Harmful use of alcohol: Excessive alcohol intake increases the risk of liver disease, some cancers, and hypertension.
- Environmental factors: Air pollution and exposure to toxic substances contribute to respiratory and cardiovascular diseases (Vichitkunakorn et al., 2025).
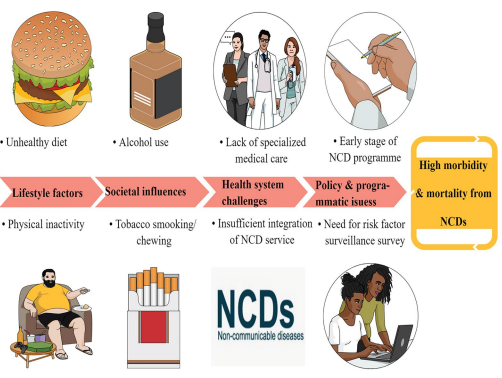
Modifiable Risk Factors:
- Modifiable behaviors, such as tobacco use, physical inactivity, unhealthy diet, and the harmful use of alcohol, all increase the risk of NCDs (WHO, 2025).
- Tobacco accounts for over 7.2 million deaths every year (including from the effects of exposure to second-hand smoke) and is projected to increase markedly over the coming years (WHO, 2025).
- 4.1 million annual deaths have been attributed to excess salt/sodium intake (WHO, 2025).
- More than half of the 3.3 million annual deaths attributable to alcohol use are from NCDs, including cancer (WHO, 2025).
- 1.6 million deaths annually can be attributed to insufficient physical activity (WHO, 2025).
Non-Modifiable Risk Factors:
- Age: As we age our risk of high BP increases. This is due to changes in the heart and blood vessels, whereby there is a loss of elasticity in the tissues found in our arteries. This loss of elasticity results in stiffening and a reduced ability to stretch, leading to increased BP.
- Genetics/Family History: Genetic predisposition plays a role in diseases like diabetes, hypertension, breast cancer, and some heart diseases. Family history can guide early screening (Peltzer et al., 2024).
- Gender: Some diseases are more common in one gender; for example, breast cancer is predominant in women, and prostate cancer in men.
- Ethnicity: People of African and Black Caribbean descent have an increase in the risk of high BP . This is said to be down to genetic predisposition that increases sensitivity to salt in the diet by as little as 1 gram of extra salt per day can increase systolic BP, the pressure exerted on blood vessels when the heart contracts, by as little as much as 5mmHg; the unit of measurement that used when determining BP.
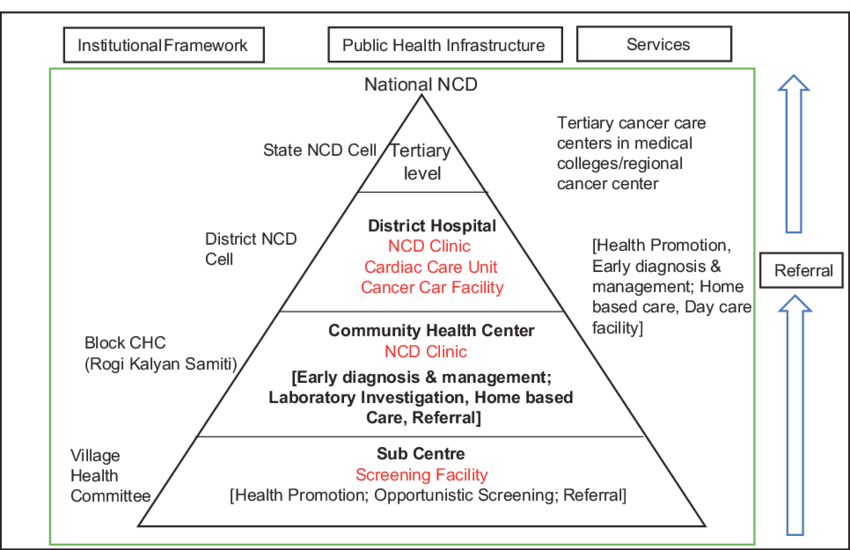
National Program for Prevention and Control of Cancer, Diabetes,
CVD and Stroke (NPCDCS)
- Prevent and control common NCDs through behaviour and life style changes,
- Provide early diagnosis and management of common NCDs,
- Build capacity at various levels of health care for prevention, diagnosis and treatment of common NCDs,
- Train human resource within the public health setup viz doctors, paramedics and nursing staff to cope with the increasing burden of NCDs, and
- Establish and develop capacity for palliative & rehabilitative care.
Quick Stats
States Covered
Delhi, Chennai, Dehradun, Gangtok
4
Urban sites
Participants
Enrolled sample size
2,400
Consented & randomized
Study Arms
Digital, WHO PEN, Control
3
Cluster RCT
Follow-up
Primary endpoint window
12 Months
Quarterly touchpoints




